December 22, 2024 - 03:16
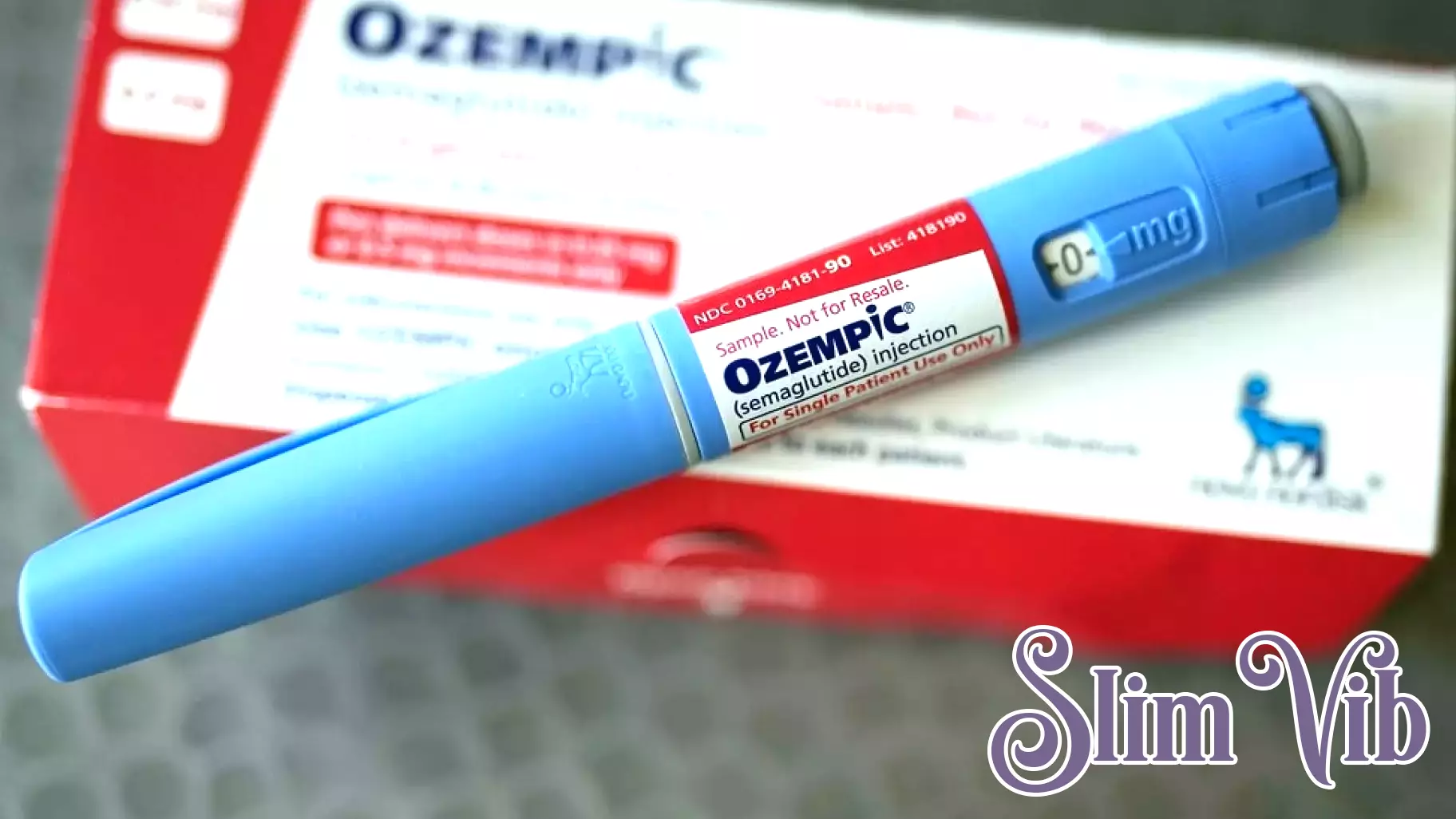
In a significant shift, Independence Blue Cross has announced that it will join a growing number of insurance providers in limiting coverage for popular weight loss medications, specifically Wegovy and Ozempic. Starting in 2025, these medications will primarily be covered for patients diagnosed with Type 2 diabetes and heart disease. This decision reflects a broader trend among insurers aiming to manage costs and ensure that medications are prescribed for medically necessary conditions.
The changes are expected to impact many individuals who have relied on these drugs for weight management purposes. As obesity rates continue to rise, the demand for effective weight loss solutions has surged, leading to increased scrutiny regarding the appropriateness of insurance coverage for these medications.
With these new restrictions, patients seeking coverage for weight loss treatments may need to explore alternative options or consider out-of-pocket expenses. This policy shift highlights the ongoing debate surrounding the role of insurance in providing access to weight management therapies and the importance of aligning treatment with specific health conditions.



